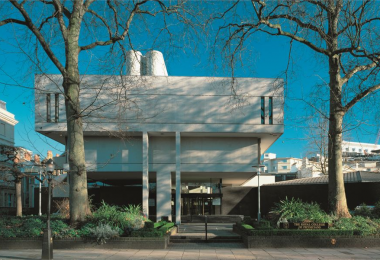
Independent charitable hospital King Edward VII’s is incorporating two new innovations to combat some of the damaging long-term side effects of breast cancer surgeries.
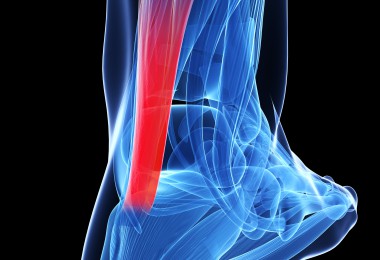
The lymphatic microsurgical healing approach (LYMPHA) reduces the risk of secondary breast cancer-related lymphedema (BCRL). This is a chronic, painful and often progressive condition where excess fluid collects in tissues, causing swelling. LYMPHA redirects waste products from the lymphatic system into the veins, enabling waste products to flow away and reducing the risk of lymphedema. The technique has been demonstrated in several studies to significantly reduce the risk of BRCL.
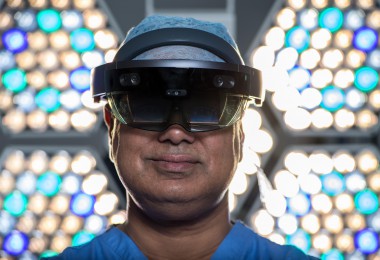
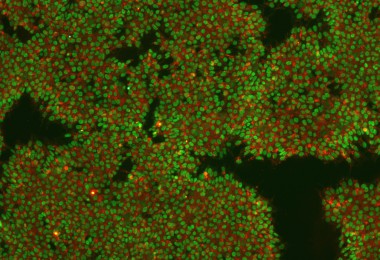
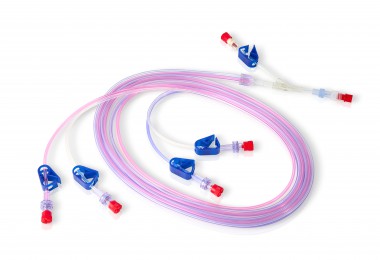
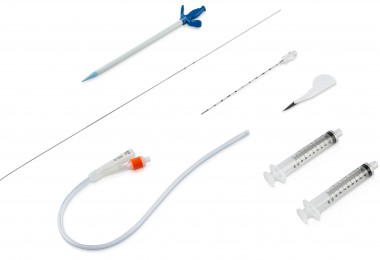
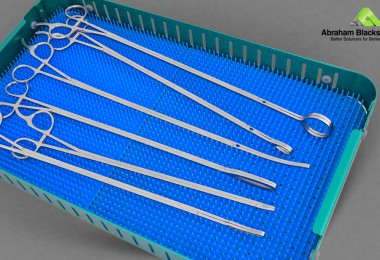
LYMPHA uses a combination of a paramagnetic tracer and fluorescent imaging (Endomagnetics and Stryker) to identify the extremely small lymphatics (~1mm) draining from the arm, and guide the surgical team at the time of operating. Consultant breast and reconstructive surgeon Mr Paul Thiruchelvamleads the team and works very closely with his colleagues Mr Navid Jallali and Miss Judith Hunter, both consultant plastic and microsurgical surgeons to undertake this complex procedure.
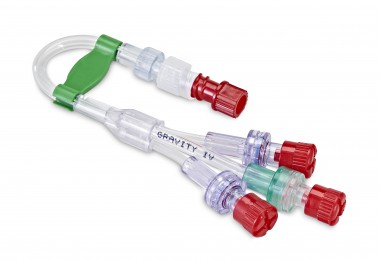
The technique has been introduced alongside deep inferior epigastric artery perforator (DIEP) flap reconstruction, a complex type of microsurgical breast reconstructive surgery. DIEP flap reconstruction transposes fat, skin, and blood vessels from the lower abdomen and moves them up to the chest to rebuild the breast mound following mastectomy.
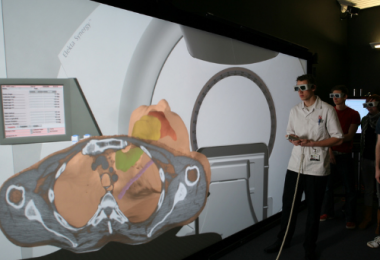
Novel, innovative quantification perfusion technology using the Stryker infra-red camera system provides quantitative information on perfusion of the skin flap (after mastectomy). In addition, it may guide the microsurgeon to select the best perfused flap and potentially reduce the incidence of fat necrosis, a condition where the tissue used to rebuild the breast dies, leading to lumpiness and unpleasant textures. Lumps caused by skin-flap necrosis not only affect the patient’s quality of life but may require further clinical assessment, and distress for the patient in the future.
Both procedures combine the expertise of King Edward VII’s breast surgeons and microsurgeons in a multidisciplinary procedure, highlighting the collaborative nature of innovation, which is so common to the historic hospital.
Mr Paul Thiruchelvam, consultant breast and reconstructive surgeon at King Edward VII’s hospital, comments: “In my career I have seen many patients suffer from the debilitating effects of lymphedema. It is incredibly rewarding to be able to work so closely with my outstanding microsurgical colleagues to reduce women’s risk of suffering from this long-term condition. At King Edward VII’s we are able to use cutting edge technology and are at the forefront of innovation to improve the lives of our patients.”
Miss Judith Hunter, Consultant Plastic and Reconstructive Surgeon and King Edward VII’s hospital, added: Lymphoedema can be very debilitating and has traditionally been a challenge to treat. Recently there has been renewed interest in microsurgical approaches to address this condition, but as with anything, prevention has turned out to be better than cure. Paul, Navid and I had the privilege to travel to Genoa a few years ago to learn from the pioneer of the LYMPHA technique, and have been delighted with our early results back in London. If a patient is having a lymph node dissection along with a mastectomy, and we are already there with the skills and equipment to perform an immediate breast reconstruction, it makes sense to offer them the LYMPHA procedure too.